Research review: prehospital TXA administration, side effects - EMS1.com
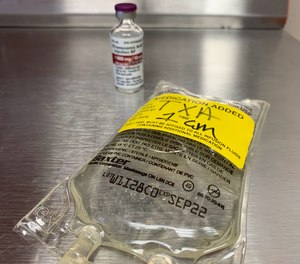
With the use of tranexemic acid [TXA] increasing dramatically, it is important to understand how it works and what role it plays in the prehospital environment.
How does coagulation work?
Coagulation is the balance between clot formation and clot destruction.
The body uses a combination of platelets and fibrin to form clots and control bleeding. To prevent inappropriate or unnecessary clotting, the body has a process to break down clots called fibrinolysis. This requires plasminogen/plasmin to bind to fibrin and dissolve it, breaking down the clot. These two mechanisms, working in tandem, create the balance necessary for normal coagulation [1].
Coagulopathy can occur when there is an imbalance between clot formation and destruction.
Coagulopathy is part of the trauma triad, the lethal spiral that includes hypothermia and acidosis, which increase mortality. There are many causes of coagulopathy in trauma. Early coagulopathy is thought to be a result of hypoxia and ischemia causing a widespread activation of the body's fibrinolytic system. This exaggerated response may shift the balance away from clot formation to clot destruction, increasing the risk of bleeding [2].
How does TXA work?
TXA is synthetically derived from lysine. Lysine, an amino acid on the surface of fibrin, is how plasmin binds to fibrin in order to break down (lyse) the clot. TXA blocks this binding site, preventing the attachment of plasmin to fibrin. TXA is referred to as an antifibrinolytic, because if plasmin can't bind to fibrin, then fibrinolysis cannot occur [2].
By preventing fibrinolysis, TXA works to prevent the coagulopathy that occurs early in the setting of massive hemorrhage.
Table 1: TXA side effects and adverse events
![Adapted from Calapai et al 2015 [15]](https://media.cdn.lexipol.com/article-images/Screen%20Shot%202022-08-04%20at%201.19.05%20PM.png?w=860&format=jpg&quality=87&crop=0%2C0%2C652%2C582)
Who should get TXA?
Trauma
Several studies have examined the use of TXA in trauma. MATTERs retrospectively described a mortality benefit in military trauma that was most significant in patients requiring >10 units of blood [3]. CRASH-2, a much larger study, involved civilian hospitals [4]. It demonstrated a decrease in mortality in trauma patients treated with TXA; the greatest benefit was in those with a blood pressure of less than 75 mmHg. As a result, the use of TXA in trauma has become widespread.
TXA in trauma appears ideally suited to prehospital administration, as there seems to be a benefit to early administration. However, clear evidence for prehospital TXA is still lacking [5]. A joint statement from ACS, ACEP and NAEMSP states, "there is not enough evidence to support or refute prehospital administration" [6].
Take home: It's reasonable to consider prehospital TXA in trauma, especially in patients with incompressible bleeds, severe hypotension or who may require massive transfusion.
Postpartum hemorrhage
Worldwide, postpartum hemorrhage [PPH] represents the leading cause of maternal death. TXA's ease of administration and availability has made it the subject of much investigation in PPH around the world. The most significant was the WOMAN trial, which enrolled over 20,000 women in 21 different countries [7]. The investigators noted that death from hemorrhage decreased in the TXA group. This led the World Health Organization to recommend the use of TXA for PPH [8]. No substantial prehospital literature exists.
Take home: It's reasonable to consider prehospital TXA in the setting of massive PPH.
Table 2: TXA applications
![Adapted from Cal et al 2015 [16]](https://media.cdn.lexipol.com/article-images/Screen%20Shot%202022-08-04%20at%201.20.12%20PM.png?w=860&format=jpg&quality=87&crop=0%2C0%2C1044%2C678)
Who should NOT get TXA
Intracranial hemorrhage
The CRASH-3 study specifically examined the use of TXA in traumatic brain injuries [9]. The study was large, and the investigators put a generally positive spin on the findings, suggesting a benefit in mild traumatic brain injury. However, the primary outcome of the study was to examine head injury deaths and TXA made no difference. Prehospital administration in moderate-to-severe head injury was also found to make no difference in outcome [10].
Multiple studies have examined the use of TXA in non-traumatic head bleeds [11]. Initially, its use in subarachnoid hemorrhage (SAH) appeared to limit rebleeding (a major cause of death in SAH), but outcomes were variable [12]. Even when TXA was examined specifically in SAH, it has never consistently improved mortality in non-traumatic head bleeds [13].
Take home: There is no demonstrated benefit with TXA in intracranial bleeding.
GI bleed
Incompressible sites, large volume blood loss and mortality risk are a few of the things that made GI bleeds seem like a natural fit for TXA administration. Early research seemed promising, but trials were small. The HALT-IT trial examined over 15,000 patients to see if TXA reduced death [14]. Not only did TXA have no effect on mortality, it increased the risk of seizure and thromboembolic events.
Take home: No demonstrated benefit with TXA in GI bleeding
TXA research summary
A large body of research on TXA exists, and while it appears to be generally safe, it does have side-effects. Very little research exists for its use in the prehospital environment. Lacking any specific evidence or recommendations, paramedics should consider TXA as an adjunctive therapy only in specific patients. Mainstays such as hemorrhage control, balanced resuscitation with blood as well as rapid transport to an appropriate facility should remain the focus of treatment.

Read more:
Calcium in hemorrhagic trauma
Reviewing the trauma lethal triad: hypothermia, acidosis and coagulopathy
- Stansfield, R., Morris, D., & Jesulola, E. [2020]. The use of tranexamic acid [TXA] for the management of hemorrhage in trauma patients in the prehospital environment: literature review and descriptive analysis of principal themes. Shock, 53[3], 277-283.
- Nishida, T., Kinoshita, T., & Yamakawa, K. [2017]. Tranexamic acid and trauma-induced coagulopathy. Journal of Intensive Care, 5[1], 1-7.
- Morrison, J. J., Dubose, J. J., Rasmussen, T. E., & Midwinter, M. J. [2012]. Military application of tranexamic acid in trauma emergency resuscitation [MATTERs] study. Archives of surgery, 147[2], 113-119.
- Roberts, I., Shakur, H., Coats, T., Hunt, B., Balogun, E., Barnetson, L., Cook, L., Kawahara, T., Perel, P., Prieto-Merino, D., Ramos, M., Cairns, J., & Guerriero, C. [2013]. The CRASH-2 trial: a randomised controlled trial and economic evaluation of the effects of tranexamic acid on death, vascular occlusive events and transfusion requirement in bleeding trauma patients. Health technology assessment [Winchester, England], 17[10], 1–79. https://doi.org/10.3310/hta17100
- Guyette, F. X., Brown, J. B., Zenati, M. S., Early-Young, B. J., Adams, P. W., Eastridge, B. J., ... & STAAMP Study Group. [2021]. Tranexamic acid during prehospital transport in patients at risk for hemorrhage after injury: a double-blind, placebo-controlled, randomized clinical trial. JAMA surgery, 156[1], 11-20.
- Fischer, P. E., Bulger, E. M., Perina, D. G., Delbridge, T. R., Gestring, M. L., Fallat, M. E., ... & Sanddal, N. D. [2016]. Guidance document for the prehospital use of tranexamic acid in injured patients. Prehospital Emergency Care, 20[5], 557-559.
- Shakur, H., Roberts, I., Fawole, B., Chaudhri, R., El-Sheikh, M., Akintan, A., ... & Loto, O. [2017]. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage [WOMAN]: an international, randomised, double-blind, placebo-controlled trial. The Lancet, 389[10084], 2105-2116.
- World Health Organization. [2017]. WHO recommendation on tranexamic acid for the treatment of postpartum haemorrhage. World Health Organization. https://apps.who.int/iris/handle/10665/259374. License: CC BY-NC-SA 3.0 IGO
- CRASH, T. [2019]. Effects of tranexamic acid on death, disability, vascular occlusive events and other morbidities in patients with acute traumatic brain injury [CRASH-3]: a randomised, placebo-controlled trial. The Lancet, 394[10210], 1713-1723.
- Rowell, S. E., Meier, E. N., McKnight, B., Kannas, D., May, S., Sheehan, K., Bulger, E. M., Idris, A. H., Christenson, J., Morrison, L. J., Frascone, R. J., Bosarge, P. L., Colella, M. R., Johannigman, J., Cotton, B. A., Callum, J., McMullan, J., Dries, D. J., Tibbs, B., Richmond, N. J., … Schreiber, M. A. [2020]. Effect of Out-of-Hospital Tranexamic Acid vs Placebo on 6-Month Functional Neurologic Outcomes in Patients With Moderate or Severe Traumatic Brain Injury. JAMA, 324[10], 961–974. https://doi.org/10.1001/jama.2020.8958
- Baharoglu MI, Germans MR, Rinkel GJ, Algra A, Vermeulen M, van Gijn J, Roos YB. Antifibrinolytic therapy for aneurysmal subarachnoid haemorrhage. Cochrane Database Syst Rev. 2013 Aug 30;2013[8]:CD001245. doi: 10.1002/14651858.CD001245.pub2. PMID: 23990381; PMCID: PMC8407182.
- Bouillon-Minois, J. B., Croizier, C., Baker, J. S., Pereira, B., Moustafa, F., Outrey, J., ... & Dutheil, F. [2021]. Tranexamic acid in non-traumatic intracranial bleeding: a systematic review and meta-analysis. Scientific Reports, 11[1], 1-10.
- Post, R., Germans, M. R., Tjerkstra, M. A., Vergouwen, M., Jellema, K., Koot, R. W., Kruyt, N. D., Willems, P., Wolfs, J., de Beer, F. C., Kieft, H., Nanda, D., van der Pol, B., Roks, G., de Beer, F., Halkes, P., Reichman, L., Brouwers, P., van den Berg-Vos, R. M., Kwa, V., … ULTRA Investigators [2021]. Ultra-early tranexamic acid after subarachnoid haemorrhage [ULTRA]: a randomised controlled trial. Lancet [London, England], 397[10269], 112–118. https://doi.org/10.1016/S0140-6736[20]32518-6
- Roberts, I., Shakur-Still, H., Afolabi, A., Akere, A., Arribas, M., Brenner, A., ... & McClelland, L. [2020]. Effects of a high-dose 24-h infusion of tranexamic acid on death and thromboembolic events in patients with acute gastrointestinal bleeding [HALT-IT]: an international randomised, double-blind, placebo-controlled trial. The Lancet, 395[10241], 1927-1936.
- Calapai, G., Gangemi, S., Mannucci, C., Minciullo, P. L., Casciaro, M., Calapai, F., ... & Navarra, M. [2015]. Systematic review of tranexamic acid adverse reactions. Journal of Pharmacovigilance, 2015.
- Cai, J., Ribkoff, J., Olson, S., Raghunathan, V., Al‐Samkari, H., DeLoughery, T. G., & Shatzel, J. J. [2020]. The many roles of tranexamic acid: an overview of the clinical indications for TXA in medical and surgical patients. European journal of haematology, 104[2], 79-87.
Comments
Post a Comment